In the intricate and critical world of healthcare, few pieces of equipment hold as much significance as the vaccine refrigerator. These specialized units are not merely cooling devices; they are meticulously engineered environments designed to safeguard the integrity and efficacy of life-saving vaccines. Maintaining the precise temperature range required for vaccine storage is paramount, as deviations can lead to irreversible damage, rendering these essential biological products ineffective and potentially compromising patient health. This comprehensive guide delves deep into the nuances of vaccine refrigerators, exploring their various types, crucial features, stringent regulatory requirements, essential maintenance practices, and the overarching importance of adhering to best practices in vaccine storage.
Understanding the Critical Role of Precise Temperature Control
Vaccines are complex biological preparations that are highly sensitive to temperature fluctuations. Exposure to temperatures outside the recommended range, whether too hot or too cold, can compromise their potency. This loss of efficacy is often irreversible and undetectable by visual inspection. Administering a compromised vaccine not only fails to provide the intended protection against disease but also erodes public trust in vaccination programs. Therefore, a reliable and meticulously monitored vaccine refrigerator is not just a piece of equipment; it is a cornerstone of public health infrastructure.
Types of Vaccine Refrigerators: Tailoring Solutions to Specific Needs
The market offers a diverse range of vaccine refrigerators, each designed to meet specific storage requirements and operational contexts. Understanding these different types is crucial for healthcare providers to make informed decisions when selecting the most appropriate unit for their needs:
- Purpose-Built Pharmaceutical Refrigerators: These are specifically designed for the storage of medications and vaccines. They typically feature precise temperature control systems, digital temperature displays, alarms for temperature excursions, and often have features like forced-air circulation to ensure temperature uniformity throughout the cabinet. These are often considered the gold standard for vaccine storage.
- Medical-Grade Refrigerators: Similar to pharmaceutical refrigerators, these units are engineered for medical applications and often include features that meet stringent healthcare standards. They prioritize temperature stability and reliability.
- Laboratory Refrigerators: While often used for a broader range of laboratory samples, certain high-quality laboratory refrigerators can meet the temperature requirements for vaccine storage. However, it’s crucial to ensure they have the necessary features like precise temperature control and monitoring.
- Domestic or Household Refrigerators (Not Recommended): Standard household refrigerators are strongly discouraged for vaccine storage. They often lack the temperature stability, consistent airflow, and monitoring capabilities essential for maintaining vaccine potency. Temperature fluctuations within these units can be significant and unpredictable, posing a serious risk to vaccine efficacy.
- Ultra-Low Temperature (ULT) Freezers: While primarily used for long-term storage of certain specialized vaccines and biological samples at extremely low temperatures (e.g., -80°C), they are a critical component of the cold chain for specific products. These require specialized handling and monitoring.
Key Features to Look for in a High-Quality Vaccine Refrigerator
Selecting the right vaccine refrigerator involves careful consideration of several crucial features that directly impact its ability to maintain optimal storage conditions:
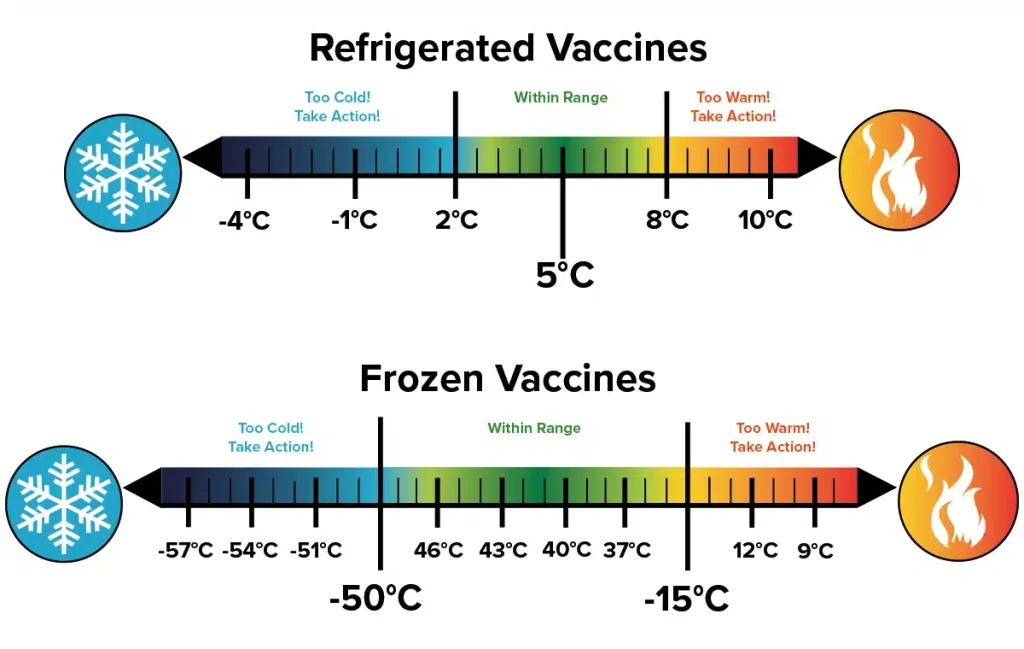
- Precise Temperature Control: The refrigerator should be capable of maintaining a consistent temperature within the recommended range (typically 2°C to 8°C or 36°F to 46°F). Look for units with accurate and reliable thermostats.
- Digital Temperature Display: An easily visible external digital temperature display allows for continuous monitoring without opening the refrigerator door, minimizing temperature fluctuations.
- Temperature Monitoring and Data Logging: Advanced units may include integrated data loggers that automatically record temperature readings at regular intervals. This data can be crucial for demonstrating compliance and identifying potential issues.
- Temperature Alarms: Audible and visual alarms that trigger when the temperature deviates outside the acceptable range are essential for prompt intervention. These alarms should alert staff to potential problems before vaccine efficacy is compromised.
- Forced-Air Circulation: A fan-driven air circulation system ensures uniform temperature distribution throughout the refrigerator cabinet, preventing hot or cold spots that can damage vaccines.
- Self-Closing Doors with Secure Latches: These features help to maintain temperature stability by minimizing the duration the door is open and ensuring a tight seal.
- Dedicated Vaccine Storage Compartments: Some refrigerators are designed with specific compartments or drawers that optimize airflow and organization for vaccine storage.
- Frost-Free Operation (with Caution): While frost-free freezers are common, frost buildup in refrigerators can sometimes indicate temperature control issues. If selecting a frost-free refrigerator, ensure it has robust temperature control mechanisms. Manual defrost models may offer more temperature stability but require regular maintenance.
- Remote Monitoring Capabilities: Some advanced systems offer remote temperature monitoring and alerts, allowing for proactive management and intervention even when staff are not physically present.
- Battery Backup for Alarms: In the event of a power outage, a battery backup ensures that temperature alarms remain functional.

Navigating the Regulatory Landscape: Compliance and Best Practices
The storage and handling of vaccines are subject to stringent regulations and guidelines established by national and international health organizations. Adherence to these standards is not just a matter of compliance; it is fundamental to ensuring vaccine safety and efficacy. Key regulatory bodies and guidelines include:
- Centers for Disease Control and Prevention (CDC): The CDC provides comprehensive guidelines on vaccine storage and handling, including recommended temperature ranges, monitoring procedures, and inventory management.
- World Health Organization (WHO): The WHO also publishes detailed guidelines on the cold chain for vaccines, particularly relevant in global health initiatives.
- State and Local Health Departments: Many state and local health departments have their own specific regulations and recommendations regarding vaccine storage.
- Professional Organizations: Organizations like pharmacy and nursing associations often provide best practice recommendations for vaccine handling and storage.

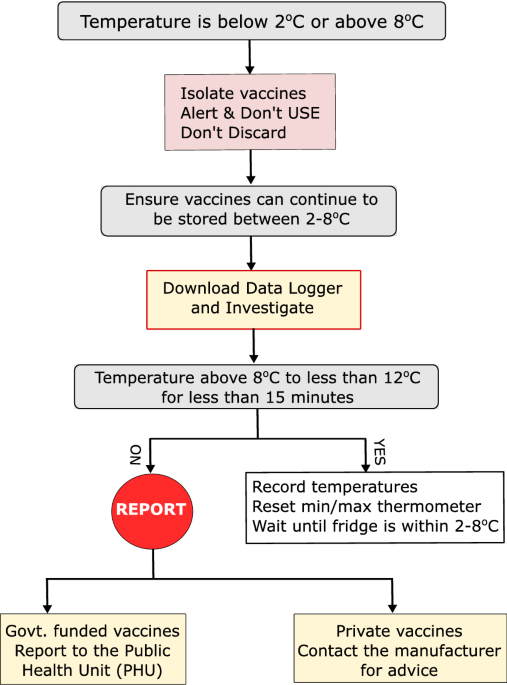
It is imperative for healthcare providers to be thoroughly familiar with and strictly adhere to all relevant regulations and guidelines pertaining to vaccine refrigerators and vaccine storage protocols. This includes maintaining detailed temperature logs, responding promptly to temperature excursions, and implementing robust inventory management systems.
Essential Maintenance for Optimal Performance and Longevity
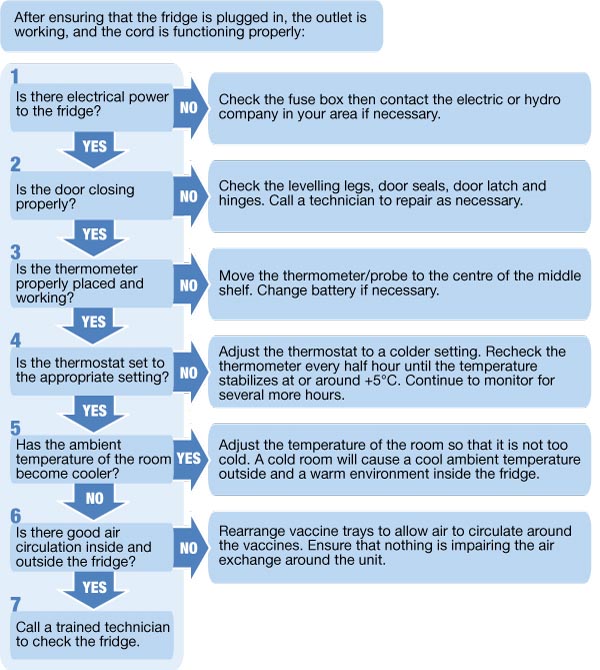
Regular and diligent maintenance is crucial for ensuring the reliable operation and longevity of a vaccine refrigerator. Neglecting maintenance can lead to temperature inconsistencies, equipment failures, and ultimately, compromised vaccines. Key maintenance practices include:
- Regular Cleaning: The interior and exterior of the refrigerator should be cleaned regularly to prevent dust buildup and maintain hygiene.
- Temperature Calibration: Periodic calibration of the temperature monitoring system ensures accuracy. Follow the manufacturer’s recommendations for calibration frequency.
- Door Seal Inspection: Regularly inspect door seals for any signs of damage or wear. A faulty seal can lead to temperature fluctuations and increased energy consumption.
- Defrosting (for Manual Defrost Models): Manual defrost refrigerators require periodic defrosting to remove ice buildup, which can impair cooling efficiency. Follow the manufacturer’s instructions for defrosting.
- Condenser Coil Cleaning: Dust and debris can accumulate on the condenser coils, reducing the refrigerator’s ability to dissipate heat efficiently. Clean the coils regularly according to the manufacturer’s recommendations.
- Professional Servicing: Schedule regular professional servicing by qualified technicians to identify and address any potential issues before they lead to equipment failure.
- Battery Backup Testing: For units with battery backups for alarms, regularly test the battery to ensure it is functioning correctly.
Best Practices for Vaccine Storage within the Refrigerator
Even with a high-quality vaccine refrigerator, proper storage practices are essential to maintain vaccine efficacy:
- Proper Organization: Arrange vaccines in a way that allows for good air circulation. Avoid overcrowding the refrigerator.
- Designated Storage Areas: Designate specific areas within the refrigerator for different types of vaccines to prevent errors.
- Avoid Storing Food or Other Non-Medical Items: Vaccine refrigerators should be used exclusively for vaccine storage to minimize the risk of contamination and temperature fluctuations.
- Do Not Store Vaccines in the Door: The temperature in the refrigerator door tends to fluctuate more than in the main compartment.
- Maintain Proper Inventory Management: Implement a system for tracking vaccine expiration dates and ensuring proper stock rotation (first-in, first-out).
- Establish Emergency Protocols: Develop and regularly practice protocols for responding to power outages, temperature excursions, and equipment failures. Ensure staff know the location of backup storage and how to transfer vaccines if necessary.
- Continuous Temperature Monitoring: Implement a system for continuous temperature monitoring, whether through manual readings or automated data logging. Review temperature logs regularly.
- Document Everything: Maintain detailed records of temperature logs, maintenance activities, and any temperature excursions and the actions taken.
The Future of Vaccine Refrigeration: Innovation and Advancements
The field of vaccine refrigeration continues to evolve, with ongoing advancements focused on enhancing efficiency, reliability, and monitoring capabilities. Innovations include more sophisticated temperature control systems, advanced data logging and analytics, remote monitoring via IoT (Internet of Things) devices, and the development of more sustainable and energy-efficient refrigeration technologies. These advancements will play a crucial role in strengthening the cold chain and ensuring the safe and effective delivery of vaccines globally.
In conclusion, the vaccine refrigerator is an indispensable piece of equipment in the healthcare ecosystem. Its proper selection, meticulous maintenance, and adherence to stringent storage protocols are paramount to safeguarding vaccine potency and ultimately protecting public health. By understanding the nuances of these specialized refrigerators and implementing best practices, healthcare providers can ensure that these life-saving biological products remain effective and contribute to a healthier future for all.